Anatomy of the Diaphragm
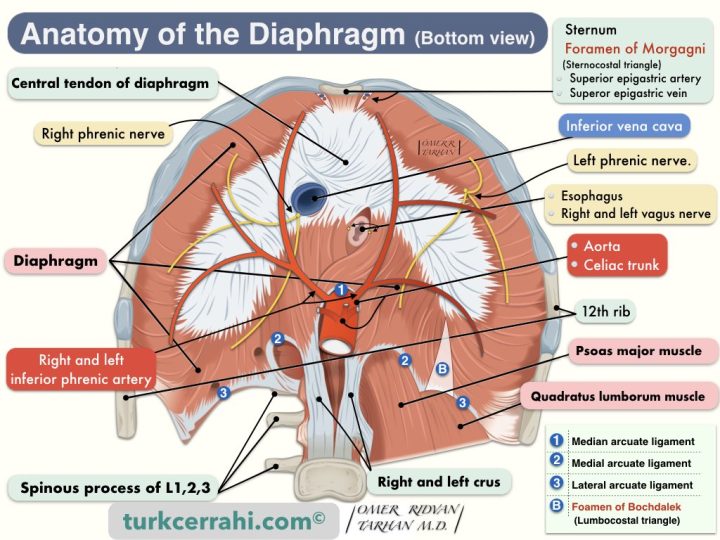
Image retrieved from Wikipedia on 28 April 2017 under Creative Commons Attribution-ShareAlike 4.0 International (CC BY-SA 4.0). Image's Page. OpenStax the copyright holder of this work. Some descriptions and labels of the image have been reorganized by turkcerrahi.com/en
- Definition
- Is the Diaphragm Striated or Smooth Muscle?
- Borders of the Diaphragm
- Crus of Diaphragm (pl. Crura)
- Diaphragmatic Openings (Hiatus) and Structures Pass-Through
- Ligaments of the Diaphragm
- Diaphragm Domes
- Blood Supply of the Diaphragm
- Innervation of the Diaphragm
- Physiology of Ventilation and Respiration
- Embryology of the Diaphragm
- Diaphragmatic Hernias
1. Definition
The diaphragm is a musculomembranous (musculotendinous) structure that separates the abdominal and thoracic (chest) cavities. The diaphragm resembles a parachute. The middle is membranous (parachute fabric), and the edges are muscles (parachute strings). The tendinous middle part of the diaphragm is called the central tendon (centrum tendineum).
2. Is the Diaphragm Striated or Smooth Muscle?
The muscle tissue that forms the sides of the diaphragm is a striated muscle (i.e., skeletal muscle). However, the diaphragm muscle and breathing normally work involuntarily (automatically). Sometimes, voluntary breathing also comes into play. For example, talking, singing, laughing, deep breathing, and whistling. Breathing is also temporarily changed by complex reflexes like yawning, sneezing, straining, belching, coughing, and vomiting.
3. Borders of the Diaphragm
The diaphragm attaches anteriorly to the xiphoid process and costal margin, and laterally to the 6th to 12th ribs. The diaphragm attaches posteriorly to the lateral, medial, and median arcuate ligaments. These ligaments attach to the body of the quadratus lumborum muscle, the psoas major muscle, and the first three lumbar vertebrae, respectively (from lateral to medial) (L1-3).
The posterior side of the diaphragm is longer than the anterior. Therefore, in the superior part of the posterior abdominal wall, the diaphragm is located.
4. Crus of Diaphragm (pl. Crura)
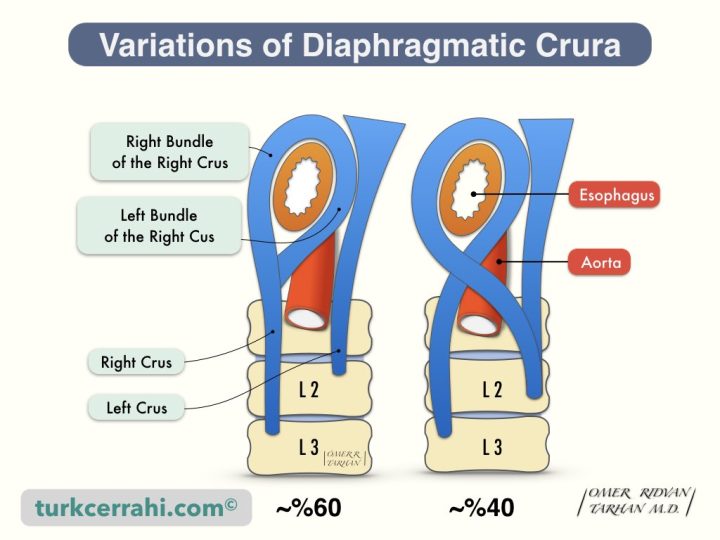
The crura of the diaphragm are two musculotendinous structures that connect the mid-posterior part of the diaphragm to the lumbar vertebrae. The right and left crus converge superiorly in front of the esophagus, so the esophagus and aorta remain between the two crus. The right and left crus are joined by a tendinous arch anterior to the aorta (median arcuate ligament).
Right Crus
The right crus is longer and wider than the left crus. The right crus attaches to the L1–3 vertebral bodies.
Left Crus
The left crus attaches to the L1–2 vertebral bodies. So the left crus is shorter than the right crus.
There are two main variations of the diaphragm crus. First, both the right and left bundles that surround the esophagus originate from the right crus (~ 60%). In another frequent variation, the right and left crus enclose the esophagus in an "8" shape (~ 40%). These variations are not associated with hiatal hernia frequency and type.
5. Diaphragmatic Openings (Hiatus) and Structures Pass-Through
Many structures pass through the diaphragm or around its edges.
Esophageal Hiatus
- Esophagus: The esophagus passes through the muscular portion of the diaphragm at the level of T10, up to 2,5 cm to the left of the midline. The esophageal hiatus is located superoanterior and slightly to the left of the aortic hiatus. The anterior and lateral borders of the hiatus are formed by the muscular arms of the diaphragmatic crura and the posterior border by the median arcuate ligament.
- Anterior and posterior vagal trunk
- Esophageal branches of the left gastric artery and vein
Hiatus of Inferior Vena Cava
The hiatus of the inferior vena cava is to the right of the central tendon of the diaphragm (centrum tendineum), at the level of T8, approximately 2.5 cm to the right of the midline.
- Inferior Vena Cava
- Right Phrenic Nerve: Phrenic nerves arise from C3-C5 on both sides. They reach the diaphragm by passing between the lungs and heart. It is both a motor and a sensory nerve. The right phrenic nerve usually crosses the diaphragm to the right of the inferior vena cava. The left phrenic nerve passes over the pericardium of the left ventricle, perforates the diaphragm, and distributes to the lower surface of the diaphragm.
Aortic Hiatus
- The aorta passes behind the diaphragm rather than through it at the level of T12. The aortic hiatus is bounded anteriorly by the median arcuate ligament, laterally by the diaphragmatic crura, and posteriorly by the body of the first lumbar vertebra.
- Thoracic Duct (Ductus Thoracicus): The thoracic duct is the largest lymphatic vessel in the body. Ductus thoracicus begins with cisterna chyli (L1-2) at the T12 level and empties into the proximal brachiocephalic vein. The thoracic duct crosses the aortic hiatus along with the azygos vein on its right. Both are anterior to the vertebral bodies and posterior to the aorta.
- Azygos Vein: Azygos vein begins in the L2-T12 interval (with the union of the lumbar and subcostal veins). It ascends in front of and to the right of the vertebral bodies. After passing through the aortic hiatus, it drains behind the superior vena cava (at the level of the right main bronchus). The azygos vein sometimes passes through the right crus.
- Hemiazygos Vein: The hemiazygos vein is the symmetrical vein of the azygos on the left. The hemiazygos vein drains into the azygos vein at the level of T9.
Foramen of Morgagni
- Right and Left Superior Epigastric Artery and Vein: The superior epigastric artery and vein are the continuations of the internal thoracic artery and vein (surgeons call the internal thoracic artery and vein the internal mammarian artery and vein, LIMA, RIMA, LIMV, RIMV). Morgagni’s hernia usually occurs through the right foramen of Morgagni (90%).
Foramen of Bochdalek
The foramen of Bochdalek is a fetal diaphragmatic opening. It is also called the lumbocostal triangle. The diaphragm closes between 8 and 10 weeks of fetal life. As a result, in healthy humans, the foramen of Bochdalek is absent (closed), and no anatomical structure passes through it. (Vincenz Alexander Bochdalek, 1801-1883, Czech Professor of Anatomy)
The base of this triangle is at the edge of the lateral arcuate ligament (level of the XIIth rib), and its apex is toward the central tendon.
Foramen Bochdalek is the source of the Bochdalek hernia, a congenital diaphragmatic hernia. The other congenital diaphragmatic hernia is the Morgagni hernia. 85% of Bochdalek hernias are on the left, and 15% are on the right (liver).
Other Structures Passing Through the Diaphragm
- The greater and lesser splanchnic nerves pass through the left crus (they originate from T5-10 and T10-11, respectively, and go to the celiac ganglion and superior mesenteric ganglion, respectively).
- Hemyazygos vein usually passes through the aortic hiatus, sometimes through the left crus.
- Right and Left Sympathetic Truncus: On both sides, they pass behind the median arcuate ligament. They extend from the base of the skull to the coccyx (on either side of the vertebral body). They are important elements of the autonomic nervous system (sympathetic).
- Left Phrenic Nerve: Phrenic nerves emerge from C3-C5 on both sides. Phrenic nerves reach the diaphragm by passing between the lungs and heart. Phrenic nerves are both motor and sensory nerves. The right phrenic nerve crosses the diaphragm (usually) to the right of the inferior vena cava. The left phrenic nerve passes over the pericardium of the left ventricle and perforates the diaphragm and is distributed on the lower surface of the diaphragm.
6. Ligaments of the Diaphragm
Median Arcuate Ligament
The median arcuate ligament separates the esophageal and aortic hiatuses. The union of the right and left crus forms the median arcuate ligament. The median arcuate ligament may be either fibrous or muscular. If it is fibrous, it is easily seen; if it is muscular, it is difficult to distinguish.
Median Arcuate Ligament Syndrome: Normally, the median arcuate ligament passes in front of the aorta at the level of L1. Lower ligament placement causes compression of the celiac artery and celiac ganglia. This leads to abdominal pain and weight loss. The median arcuate ligament is formed by the fusion of the right and left crus with a tendinous arch anterior to the aorta.
Medial Arcuate Ligament
The medial arcuate ligaments are located to the right and left of the median arcuate ligament. The psoas major muscle passes behind the diaphragm. The tendinous arch where the diaphragm attaches to the psoas major muscle fascia is called the medial arcuate ligament.
The lateral leg of the medial arcuate ligament attaches to the spinous process of L1, and the medial leg to the vertebral bodies of L1-3 with the right crus. The sympathetic chain runs behind the medial arcuate ligament.
Lateral Arcuate Ligament
The lateral arcuate ligament is a tendinous arch that connects the diaphragm to the quadratus lumborum muscle fascia. The lateral arcuate ligament attaches to the 12th rib, while the medial leg attaches to the transverse process of L1. The subcostal nerve, artery, and vein pass behind the lateral arcuate ligament.
7. Diaphragm Domes
The diaphragm is a musculomembranous (musculotendinous) structure with two domes that separates the abdominal and thoracic (chest) cavities.
The right dome is formed by the liver, the right kidney, and the adrenal gland; the left dome is formed by the spleen, the fundus of the stomach, and the left kidney and adrenal gland. The right dome is slightly higher. In expiration, the right dome is at the level of the 5th rib, and the left dome is at the level of the 5th intercostal space. During inspiration, the striated (skeletal) muscles on the outside of the diaphragm contract, and the center tendon is pulled down like a parachute.
8. Blood Supply of the Diaphragm
- The superior surface of the diaphragm
- Two branches of the internal thoracic arteries are; pericardiophrenic artery and the musculophrenic artery.
- Superior phrenic arteries arising from the thoracic aorta
- Intercostal arteries.
- The inferior surface of the diaphragm
- Inferior phrenic arteries arising from the abdominal aorta. The main blood supply occurs with these arteries.
Veins accompany arteries both above and below the diaphragm.
9. Innervation of the Diaphragm
The main nerves of the diaphragm are the right and left phrenic nerves. The phrenic nerves arise from C3-C5 on both sides. They reach the diaphragm by passing between the lungs and heart. The phrenic nerves are both motor and sensory nerves. The right phrenic nerve usually crosses the diaphragm to the right of the inferior vena cava. The left phrenic nerve passes over the pericardium of the left ventricle, perforates the diaphragm, and branches on the inferior surface of the diaphragm.
There are also sensory fibers in the peripheral region (going to the 7th-12th intercostal nerves).
10. Physiology of Ventilation and Respiration, Control of Ventilation (Breathing)
The terms "respiration" and "ventilation" are sometimes used interchangeably. So let's separate the two first.
Respiration refers to the exchange of oxygen and carbon dioxide between the atmosphere and the whole body (cells), including ventilation. In aerobic respiration, oxygen is used to oxidize organic fuel molecules (i.e., glucose), providing a source of energy (i.e., ATP), as well as carbon dioxide and water.
Ventilation means an exchange of air. Pulmonary ventilation is the physical exchange of air between the lungs and the external environment (atmosphere, etc.). Alveolar ventilation is actually a part of pulmonary ventilation, which is the exchange of gas between the alveoli and the external environment. Thus, the oxygen that comes from the atmosphere to the alveoli passes into the blood, and the carbon dioxide that passes from the blood to the alveoli is expelled.
The most important function of pulmonary ventilation (breathing) is blood gas homeostasis (balance). In other words, it is the adjustment of the partial pressure of oxygen and carbon dioxide in the arterial blood (PO2 and PCO2). The control of ventilation means the control of the air entering the lungs and the breathing rate. In most cases, the partial pressure of carbon dioxide (PCO2) determines the respiratory rate.
Arterial Blood Gas Sensors
- Sensors in the aortic and carotid bodies measure PO2 and PCO2.
- The anterior and lateral surfaces of the medulla oblongata in the brainstem measure PCO2 and pH of the cerebrospinal fluid (CSF).
The nerves transmit the information from these sensors to the respiratory center in the brainstem. The respiratory center is located in the reticular formation and other parts of the brainstem. The respiratory center controls the respiratory muscles (especially the diaphragm and intercostal muscles).
11. Embryology of the Diaphragm
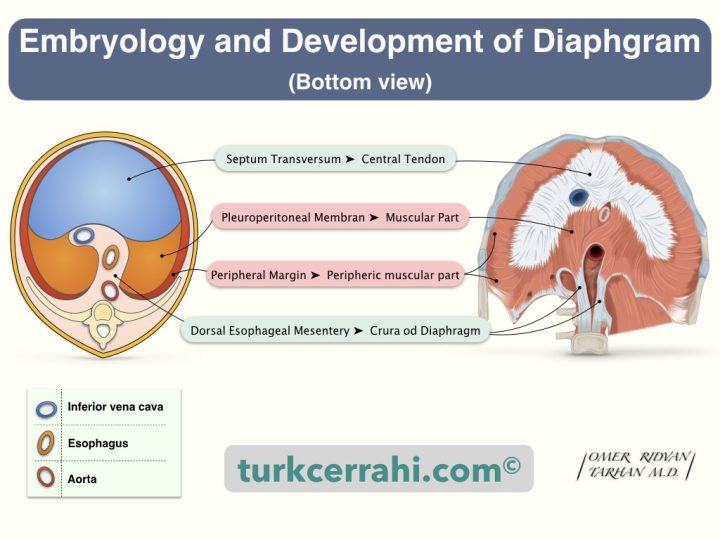
Diaphragm embryology should be known to understand congenital diaphragmatic hernias. The diaphragm develops from four structures:
- Transverse septum (anterior)
- Pleuroperitoneal membranes (posterior-lateral)
- Dorsal esophageal mesentery (mesoesophagus)
- Peripheral margin (muscular body wall).
Transverse Septum (Septum Transversum)
Two main structures develop from the transverse septum: the diaphragm (central tendon) and the ventral mesentery of the foregut (lesser omentum). The transverse septum derives from mesenchyme. The mesenchyme develops from the mesoderm, which is one of the three main germ layers in the embryo. The germ layer is any of three primary cell layers formed in the earliest stages of embryonic development, consisting of the endoderm (inner layer), the ectoderm (outer layer), and the mesoderm (middle layer).
Pleuroperitoneal Membranes
The pleuroperitoneal membranes are a pair of membranes (on the right and left) that gradually separate the pleural and peritoneal cavities. Pleuroperitoneal membranes arise from the dorsolateral (posterior-lateral) aspect of the body wall. The free margins elongate and fuse with the dorsal mesentery of the esophagus and the transverse septum. Following fusion, myoblasts (myocyte-muscle cell precursors) in the transverse septum infiltrate the pleuroperitoneal membrane and form the diaphragm muscle.
Dorsal Esophageal Mesentery
The dorsal esophageal mesentery (mesoesophagus) fuses with both the transverse septum and the pleuroperitoneal membrane. The esophageal mesentery forms the mid-posterior part of the diaphragm. Diaphragm crus develops from growing muscle fibers within the esophageal mesentery.
Peripheral Margin
In the 9th and 12th weeks, the pleural cavities enlarge and fuse with the lateral body walls. Body wall tissues also differentiate and develop medially (pleuroperitoneal membrane) to form the peripheral part of the diaphragm. Extensions of the pleural cavities to the body walls form the costodiaphragmatic sinuses (recesses).
12. Diaphragmatic Hernias
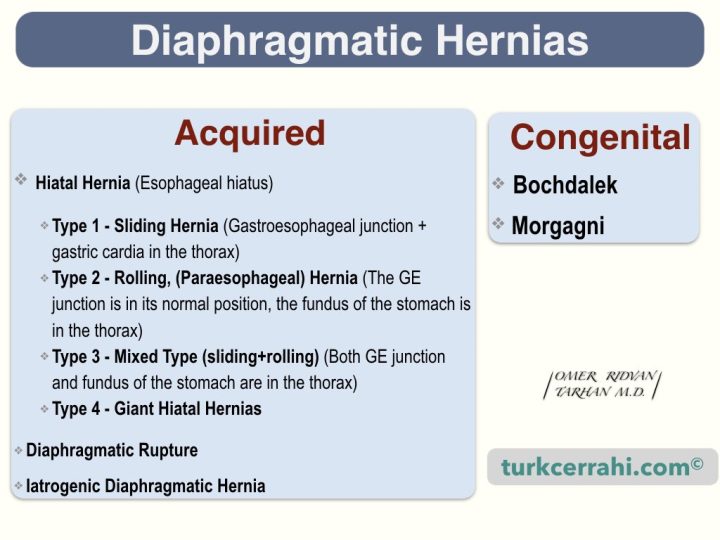
Acquired Diaphragmatic Hernias
- Hiatal Hernia (through the esophageal hiatus)
- Type 1, sliding hernia (gastroesophageal junction + gastric cardia in the thorax)
- Type 2, rolling (paraesophageal) hernia (The GE junction is in its normal position, the fundus of the stomach is in the thorax)
- Type 3, mixed type, sliding+rolling (both the GE junction and the stomach fundus are located in the thorax).
- Type 4, giant hiatal hernias: the GE junction is in its normal position; most of the stomach, colon, omentum, and spleen are in the thorax.
- Diaphragmatic Rupture: Usually occurs with penetrating injury. The hernia may enlarge and give symptoms months and years later.
- Iatrogenic Diaphragmatic Hernia: Due to previous abdominal and thoracic surgeries; such as esophagectomy, gastrectomy, nephrectomy, lung lobectomy, and liver resections.
Congenital Diaphragmatic Hernias
There are two types of congenital diaphragmatic hernias.
- Morgagni hernia
- Bochdalek Hernia
Morgagni Hernia
The Morgagni hernia occurs just to the right and behind the sternum (remember, the inferior epigastric artery and vein pass through the sternocostal triangle). Morgagni hernias are usually small, and one-third are symptomatic. Morgagni hernias can be detected in adulthood as well. They contain the omentum, the colon, and the stomach.
Bochdalek Hernia
The Bochdalek hernia is posterior to the diaphragm and usually to the left (85%), because the left pleuroperitoneal canal (diaphragm) closes later. The intestines, as is well known, develop outside of the abdomen and then return to the inside. If the pleuroperitoneal membrane is not completely closed when the intestines return to the abdomen (10th week), the intra-abdominal organs pass into the thorax. That is why the child is born with pulmonary hypoplasia. Occasionally, retroperitoneal organs (spleen and kidney) may also pass into the thorax.