Anatomy of the Esophagus
- Introduction
- Three Parts of the Esophagus
- Three Anatomical Constrictions of the Esophagus
- Layers of the Esophagus
- Abdominal Esophagus and Gastroesophageal Junction
- Anatomical Relations of the Abdominal Esophagus
- Crus of Diaphragm (pl. Crura)
- Esophageal Hiatus and Its Contents
- Phrenoesophageal Ligament - Membrane - Fascia (Laimer's Membrane - Band - Fascia)
- Esophageal Blood Supply, Venous, and Lymphatic Drainage
- Innervation (Nerves) of the Esophagus
- Esophageal Physiology
1. Introduction
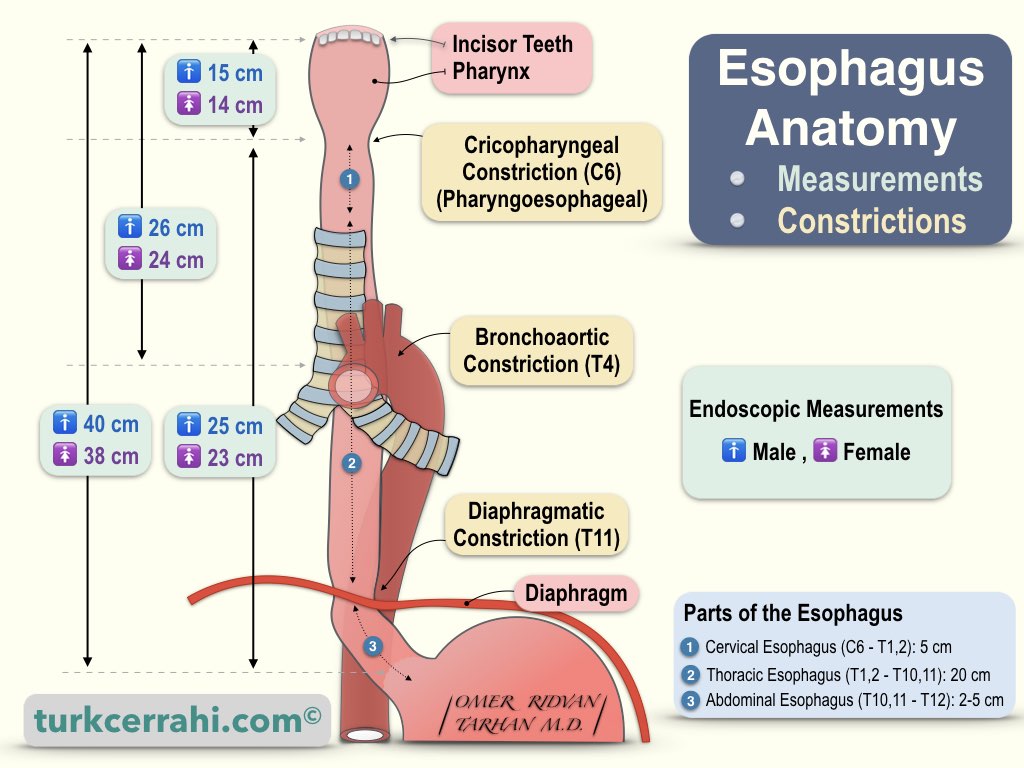
The esophagus is a muscular (smooth muscle) tube that connects the pharynx in the neck (pharynx, C6) and the stomach in the abdomen (cardia, T11). Its average length is 25-30 cm. The average distance from the incisors to the cardioesophageal junction is 40 cm in men and 37 cm in women (endoscopic measurement).
The esophagus descends behind the trachea and heart, along the front of the vertebral bodies. The esophagus generally runs through the midline but deviates to the left in two places, the first as it passes behind the aorta and the second as it passes through the esophageal hiatus (deviates to the left and anteriorly).
2. Three Parts of the Esophagus
- Cervical Esophagus: The part between the 6th cervical vertebra and the 1st-2nd thoracic vertebrae is about 5 cm long.
- Thoracic (Mediastinal) Esophagus: It starts from the 1st-2nd thoracic vertebrae, extends to the esophageal hiatus in the diaphragm, and is 20 cm long.
- Abdominal Esophagus: The part of 2-5 cm extends from the hiatus to the cardia.
3. Three Anatomical Constrictions of the Esophagus
- Cricopharyngeal or Pharyngoesophageal Constriction (Cervical Constriction ~ 1.5 cm) is the narrowest part of the esophagus, the part behind the cricoid cartilage, at the level of the cricopharyngeal muscle. This is also where the esophagus connects to the pharynx (Diameter 1.7 x2 .3 cm according to Skandalakis).
- Broncho-aortic Constriction (Thoracic Constriction ~ 1.6 cm) is where the aortic arch and left main bronchus cross the esophagus (in Gray's anatomy, the aortic arch and left main bronchus are counted as two separate stenosis, both appear as single stenosis on barium radiographs).
- Aortic Constriction (Diameter is 1.9 x 2.3 cm according to Skandalakis.)
- Bronchial Constriction (Diameter is 1.7 x 2.3 cm according to Scandalakis.)
- Diaphragmatic Constriction (Abdominal Constriction ~ 1.6-1.9 cm) is in the diaphragm, where it passes through the esophageal hiatus (2.3 cm in diameter according to Scandalakis).
The clinical significance of esophageal constrictions: Ingested foreign bodies are stuck in these constrictions, corrosive substances cause more burns in these constrictions (slowing the passage), and there is difficulty passing through these areas in endoscopy.
4. Layers of the Esophagus
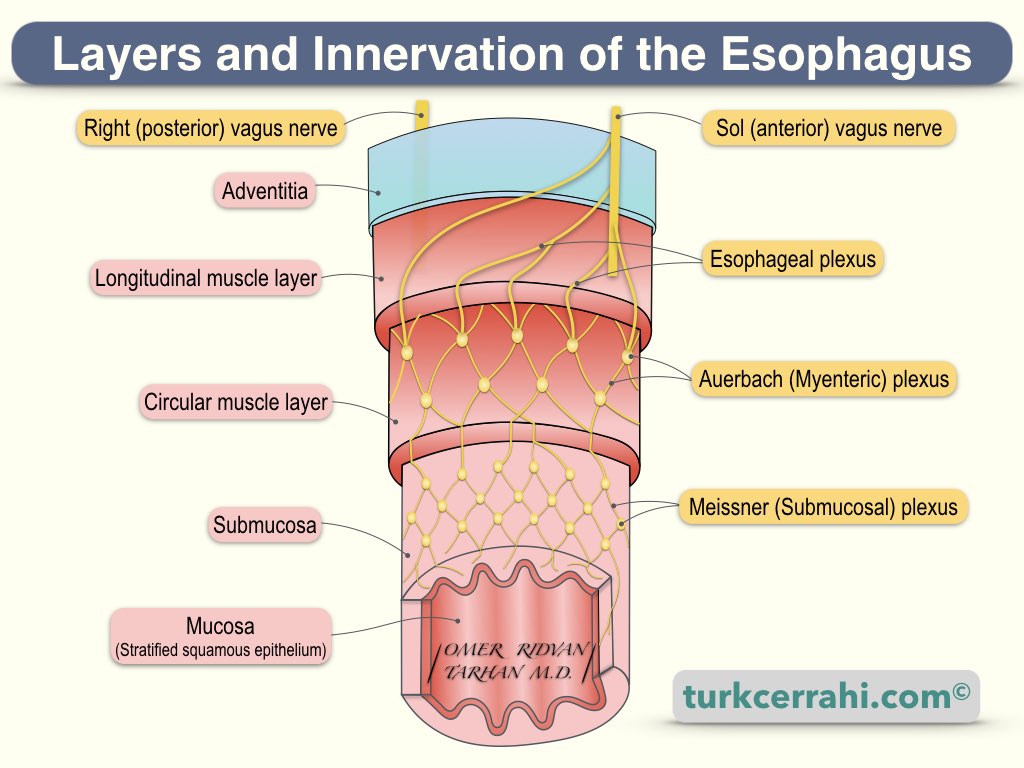
The mucosa is the innermost layer of the esophagus. It is a thick, nonkeratinized (soft), stratified squamous epithelium. It is a continuation of the oropharyngeal mucosa.
The submucosa is loose connective tissue. The thick submucosa is the strongest layer of the esophagus (The surgeon can rely on this layer for anastomosis)
Muscle Layer of the Esophagus: The esophagus has two muscle layers: an inner circular muscle layer and an outer longitudinal muscle layer. The upper quarter part is striated muscle (voluntary), and the second 1/4 is composed of striated and smooth muscle fibers (involuntary). The remaining lower half is made up entirely of smooth muscle.
Adventitia: Serosa is absent in the cervical and mediastinal esophagus. Instead, there is loose and weak connective tissue (adventitia). Adventitia does not contribute to the stability of anastomosis.
Esophageal motility disorders involve smooth muscles in the lower third. If a surgical esophageal myotomy is to be performed, it is necessary and sufficient to make the incision along this part (the lower third).
5. Abdominal Esophagus and Gastroesophageal Junction
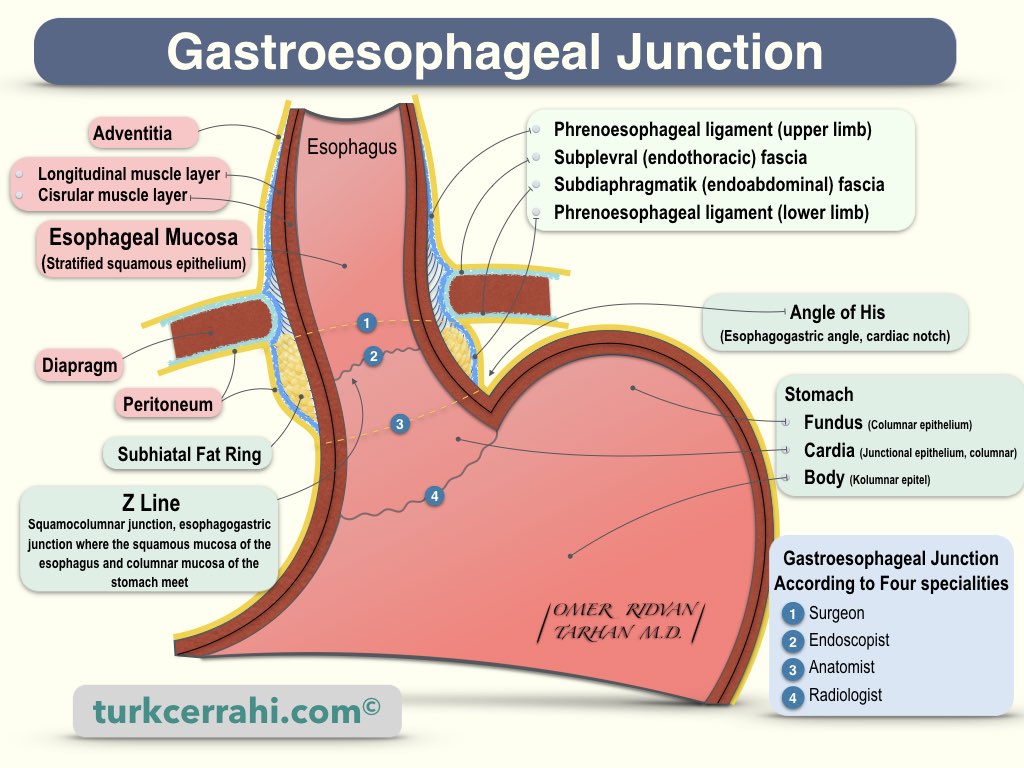
The gastroesophageal junction is defined differently on the inside (endoscopist, radiologist) and outside (surgeon, anatomist).
External Junction is just below the diaphragm (at the T11 - T12 level). The cardiac (or cardial) notch (Angle of His) is considered the border. The abdominal esophagus is usually 0.5 - 2.5 cm long and may extend up to 7 cm (between the diaphragm and gastroesophageal junction). Only the anterior and left sides of the abdominal esophagus are covered with peritoneum.
Internal Junction (Histological Junction, Z Line, Ora Serrata): The internal junction is the histological boundary between stratified squamous epithelium and columnar epithelium (gastric and esophageal mucosa, respectively). Normally, the inner junction is considered 1-2 cm superior to the outer junction. However, since the submucosal connective tissue is very loose here, the mucosa can be displaced up and down.
Cardiac Sphincter: The cardia has a sphincter mechanism that allows food to pass but prevents reflux. According to some authors, the circular muscles here are slightly thickened. However, the things that prevent reflux are
- The His angle (the angle where the esophagus enters the stomach),
- The diaphragm acts as a clamp,
- The plugging effect of the loose esophageal mucosa (mucosal rosette),
- The phrenoesophageal membrane, and the sling-shaped oblique stomach muscles (the innermost muscular layer of the stomach).
6. Anatomical Relations of the Abdominal Esophagus
- Anteriorly: Left lobe of the liver and left vagal trunk.
- Posteriorly: Right or both diaphragmatic crus, inferior phrenic artery, aorta.
- Right: The caudate lobe of the liver.
- Left: Gastric fundus.
7. Crus of Diaphragm (pl. Crura)
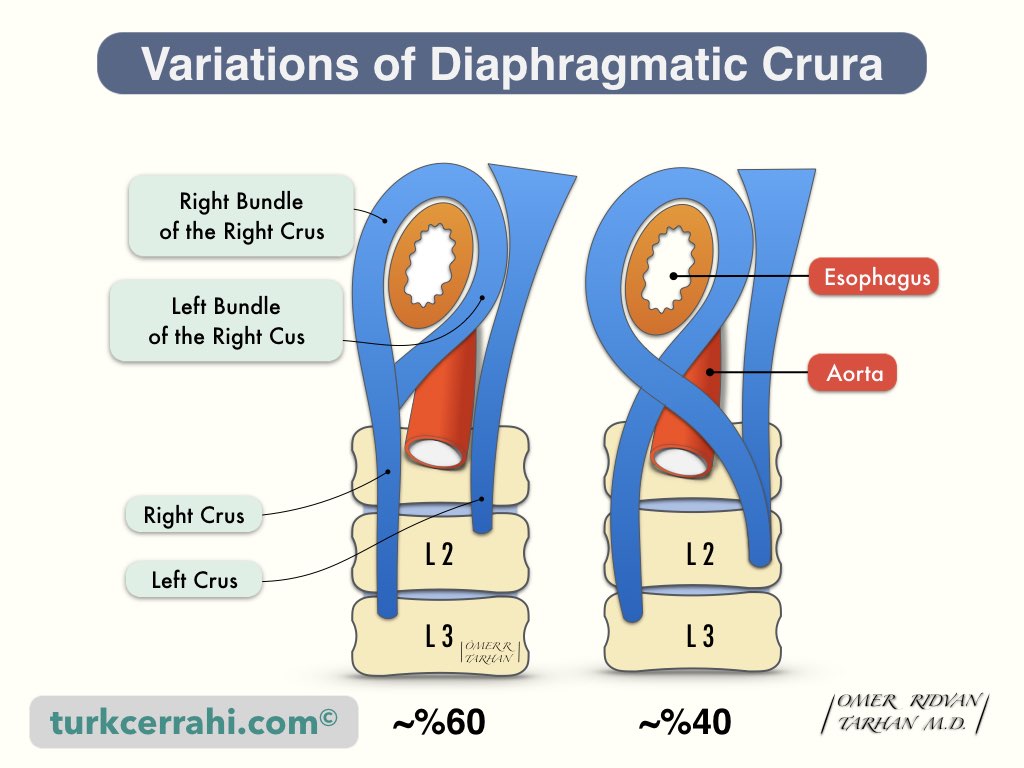
The diaphragm cruses (crura) are two musculotendinous structures that connect the posterior-medial part of the diaphragm to the lumbar vertebrae. The right and left crus merge in front of the esophagus in continuity. Thus, the esophagus and aorta remain between the two crus. A tendinous arch (median arcuate ligament) connects the right and left crus in front of the aorta.
- The right crus (crus dexter) is longer and wider. It attaches to the L1-3 vertebral bodies.
- The left crus (crus sinistrum) attaches to the L1-2 vertebral bodies, therefore it is shorter.
There are two common variations of the diaphragm crura. In the first, the right crus is the origin of both the right and left bundles that surround the esophagus (60%). Another common variation is for the right and left crus to form an "8" shape around the esophagus (40%). These variations are not related to the frequency and type of hiatal hernia.
8. Esophageal Hiatus and Its Contents
- The esophagus crosses the diaphragm at the T10 level, no more than 2.5 cm to the left of the midline. It passes through the muscular parts of the diaphragm crus. Approximately 60% of the medial and lateral fibers of the right crus (bundle) surround the esophagus, 40% of the right and left crus are crossed as 8 and the esophagus passes between them.
- Right and Left Vagus Nerve
- Esophageal Branches of left gastric artery and vein.
9. Phrenoesophageal Ligament - Membrane - Fascia (Laimer's Membrane - Band - Fascia)
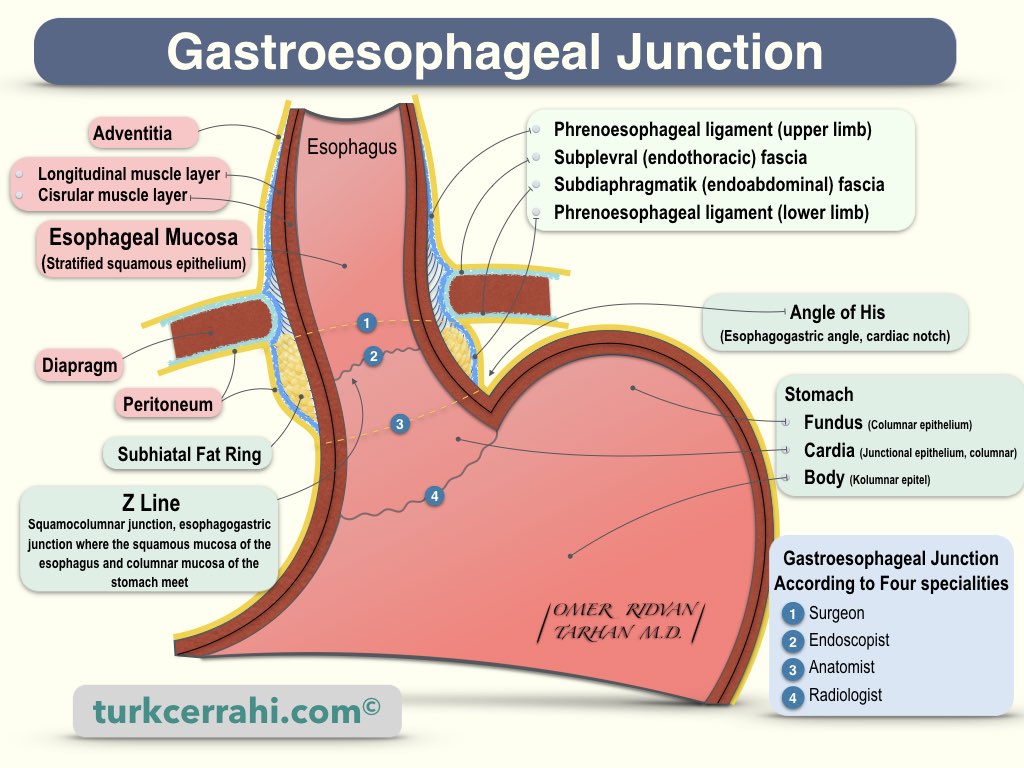
The phrenoesophageal ligament is an important part of the hiatus, which is a strong, flexible, and airtight structure that connects the esophagus to the diaphragm. This airtight structure consists of:
- Pleura
- Subpleural (endothoracic) fascia
- Phrenoesophageal ligament (fascia)
- Infra (sub) diaphragmatic extension of the fascia transversalis (endoabdominal fascia)
- Peritoneum
The pleura and peritoneum provide airtightness. Despite the difference in pressures between the abdomen and the thorax, this airtight structure prevents esophageal and stomach displacement into the thorax. Abdominal pressure is higher than thoracic pressure (+6 mmHg and -6 mmHg, respectively). This structure is also flexible, allowing food passage and diaphragm movement during respiration.
In childhood, the phrenoesophageal ligament is weaker, and in adulthood, it becomes stronger. In adulthood, adipose tissue accumulates circumferentially just below the hiatus (sub-hiatal and subperitoneal fat rings). The phrenoesophageal ligament is absent in hiatal hernia patients.
By dissecting the peritoneum and phrenoesophageal ligament on the left anterolateral side of the esophagus, the cardia and abdominal esophagus can be mobilized.
10. Esophageal Blood Supply, Venous, and Lymphatic Drainage
- Arterial Supply
- The cervical esophagus is supplied by the inferior thyroid artery,
- The thoracic esophagus is supplied by the bronchial arteries, aorta, and right intercostal arteries.
- The abdominal esophagus is supplied by the left gastric artery and the phrenic artery.
- Venous drainage: Azygos vein and thin branches joining the hemiazygos vein, esophageal branches joining the left gastric artery in the abdomen.
- Lymphatic drainage takes place mainly in the longitudinal plane.
11. Innervation (Nerves) of the Esophagus
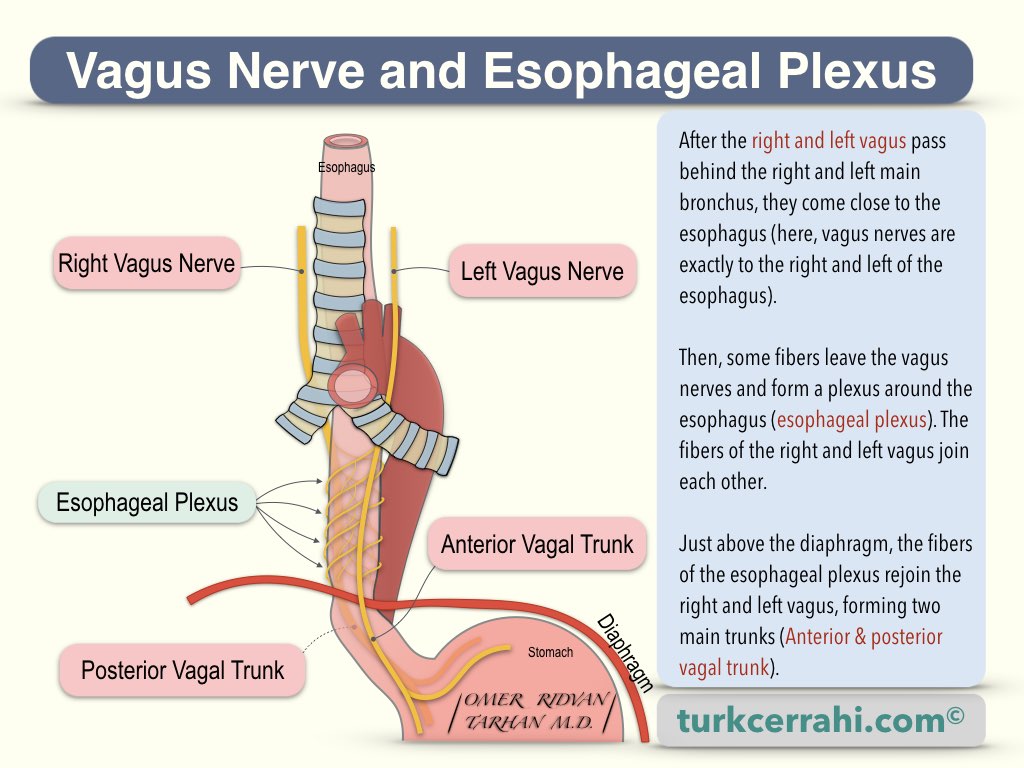
The parasympathetic innervation of the pharynx and esophagus is provided by fibers originating from the vagus nerve (efferent fibers). These fibers synapse with the myenteric and submucosal plexuses.
Sensory innervation of the esophagus is provided by vagus nerves, truncus sympathicus, and afferent fibers to the splanchnic nerves. Afferent fibers to the vagus carry information about physiological events and reflexes. Afferent fibers also carry pain sensations to the truncus sympathicus and splanchnic nerves.
The anterior vagal trunk is a continuation of the left vagus nerve (cranial nerve X, CN X) that runs anterior to the esophagus.
The posterior vagal trunk is a continuation of the right vagus (cranial nerve X, CN X), which runs right posterior to the esophagus and is thicker than the anterior vagal trunk.
12. Esophageal Physiology
The food pushed down from the oropharynx is sent to the stomach in approximately 9 seconds with primary peristaltic waves at a speed of 2-4 cm/sec. After the food enters the stomach, secondary waves initiate, which provide the cleansing function.
Swallowing
The mouth and hypopharynx form the upper third of the route from the mouth to the stomach, and the lower 2/3 is the esophagus. In this way, some pistons push the food and valves prevent it from backflow (reflux). The tongue and pharynx are pistons (pushers), while the soft palate, epiglottis, and cricopharyngeal muscle act as valves. Furthermore, the peristaltic movement of the esophagus works like a screw pump, and the valve of this pump is the lower esophageal sphincter (LES). Disruption of these pumps causes difficulty swallowing (dysphagia), while disruption of the valves causes regurgitation and gastroesophageal reflux.
Swallowing Reflex
Once swallowing has begun, a series of events follow one another as an involuntary reflex, like a Mexican wave, and swallowing takes place.
- Elevation of the tongue,
- The tongue goes backward,
- Elevation of the soft palate,
- Elevation of the hyoid bone,
- Elevation of the larynx,
- The epiglottis bends to close the larynx entrance.
All this happens in 1.5 seconds.
Esophageal Phase
After swallowing, the esophageal phase begins. The esophageal circular muscles contract in an organized fashion, pushing food into the stomach (primary peristaltic contraction, similar to a screw pump or the auger of a meat grinder). The pressure in the thorax is -6 mm Hg, and the pressure in the abdomen (stomach) is +6 mm Hg (the pressure gradient is 12 mm Hg). Esophageal peristalsis has to overcome this pressure difference as well. Primary peristaltic waves (contractions) reach the stomach about 9 seconds, after the initiation of swallowing. The speed of the peristaltic wave is 2-4 cm/sec. The contraction pressure where the peristaltic wave passes is 30-120 mm Hg (radial, occlusive, intraluminal pressure). In the case of repeated swallows, the primary peristaltic wave does not develop after each swallow. A certain time interval is required for a new peristaltic wave. Primary peristaltic waves are initiated by the swallowing center in the medulla (signal is transmitted by the vagus nerve). Stimulation of esophageal receptors is not required for primary waves.
When the esophagus distends, esophageal receptors stimulate the swallowing center (via afferent nerves), resulting in secondary waves. In other words, secondary waves occur as a result of esophageal distension and clear remaining food in the esophagus despite the primary wave.
Although the occlusive (radial) pressures in the esophagus are high during peristalsis, the propulsive force is not as strong. A 5-10 gram food can be propelled against gravity by the propulsive force. In other words, swallowing more than 5-10 grams of food in an upside-down position can cause a person to choke.
Lower Esophageal Sphincter (LES)
The lower esophageal sphincter (LES) acts as a barrier between the esophagus and the stomach, preventing reflux of the stomach contents (acid, bile, and food) into the esophagus.
There is no true sphincter structure like the pyloric sphincter at the gastroesophageal junction. Prevention of reflux is related to the architecture (design) of the gastroesophageal junction. Normally, the gastroesophageal junction is closed (the architecture of the gastric cardia creates a high-pressure zone). With swallowing, the LES also relaxes. When the esophageal peristalsis ends, the LES closes again. Relaxation of the lower esophageal sphincter may result in reflux if swallowing is not followed by adequate esophageal peristalsis.
Therefore, there are three components of the antireflux mechanism in humans.
A properly functioning lower esophageal sphincter
Properly functioning esophageal peristalsis (clearance)
Adequate gastric reservoir (overeating causes reflux).
If any of these three are compromised, the esophageal mucosa is exposed to stomach contents (acid and bile). This causes mucosal damage (esophagitis).