Anatomy of the Rectum and Anal Canal
- Anatomy of the Rectum
- Anatomy of the Anal Canal
- Anal Sphincters and Muscle Layers of the Anal Canal
- Anal Channel Encyclopedia
- Anus
- Surgical Anal Canal
- Anatomical Anal Canal
- Dentate Line (Pectinate Line)
- Anocutaneous Line (Intersphincteric Groove, White Line, Hilton's White Line)
- Anal Verge (Anal Margin)
- Anoderm
- Anal Pecten
- Columns of Morgagni (Anal Colons, Rectal Colons)
- Morgagni Sinuses (Anal Sinus, Rectal Sinus)
- Anal Crypts
- Anal Glands
- Anal Valves
- Anal Papilla (Hypertrophied Anal Papilla)
- Transitional Epithelium (Transitional Zone, Pecten)
- Pelvic Floor and Pelvic Diaphragm
- Arteries of the Rectum and Anal Canal
- Veins of the Rectum and Anal Canal
- Lymphatic Drainage of the Rectum and Anal Canal
- Innervation of the Rectum and Anal Canal
- Differences in the Anal Canal Above and Below the Dentate Line
- Defecation Physiology
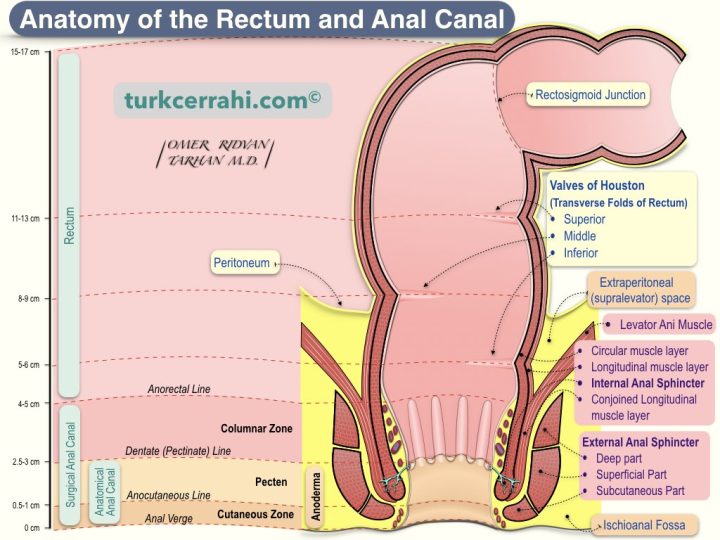
1. Anatomy of the Rectum
The rectum begins after the sigmoid colon and ends at the anus, measuring 12–15 cm long. In the rectum, taeniae, haustrations, and epiploic appendices are absent. It was given the Latin name "rectum intestinum," which means "straight intestine," due to the lack of haustrations. When surgically mobilized, the rectum elongates by 3-5 cm.
According to anatomists, the rectum begins at the SIII level, and according to surgeons, it starts at the sacral promontory. The rectum terminates at the anorectal junction. The anorectal junction is the level of the puborectal and pelvic floor muscles from the outside and the dentate line from the inside.
There are three mucosal folds in the rectum called Houston’s valve (transverse folds of the rectum). Crescent-shaped folds are located in the upper left, middle right, and lower left. These valves are located at the following distances from the anal verge in sigmoidoscopy: 4–7 cm, 8–10 cm, and 10–12 cm. The rectum is broader in its central part (rectal ampulla).
2. Anatomy of the Anal Canal
The anal canal is the last part of the large intestine, measuring 4-5 cm. The anal canal is between the rectum and the anal verge (anal orifice, anus). The anal canal allows gas and stool retention (continence). The anal canal is closed except during defecation, and the internal and external anal sphincters provide resting pressure. Thus, the involuntary escape of solid and liquid stool and gas is prevented.
To avoid confusion, we need to clarify the beginning of the anal canal. There are two main definitions of the beginning of the anal canal.
Surgical Anal Canal Definitions
- The anal canal starts at the levator ani and ends at the anal verge.
- The anal canal starts from the anorectal junction (anorectal ring) and ends at the anal verge (Schwartz).
- The anal canal starts where the rectal ampulla ends (narrows) and ends at the anal verge (Gray).
Anatomical Anal Canal Definition: The Anal canal starts from the dentate line and ends at the anal verge (anal margin).
If you notice, the starting points of the anal canal in the surgical anal canal definitions are actually the same, and they are projections of each other. As a result, the surgical anal canal is slightly longer than the anatomical anal canal. Unless we specify otherwise, we will use the surgical anal canal definition.
Anal Sphincters and Muscle Layers of the Anal Canal
Three muscle layers surround the anal canal. The inner two layers are the circular smooth muscle layer and the outer longitudinal smooth muscle layer, as in many parts of the gastrointestinal tract. The outermost is the external anal sphincter.
Internal Anal Sphincter.
The thickening of the circular smooth muscle layer forms the internal anal sphincter. The longitudinal muscle layer is the continuation of the colon taeniae. The colon's longitudinal (external) muscle layer is organized into three bands (120 degrees apart). The taeniae begin at the appendix's base and continue in three bands up to the rectum. The taeniae disperse in the rectum and wrap around the rectum and anus. In many sources, the longitudinal muscle layer is often ignored and not shown in illustrations related to the anatomy of the anal canal. Only the internal and external anal sphincters are mentioned.
External Anal Sphincter
The external anal sphincter is the outermost (third muscle) layer of the anus. The external anal sphincter is a striated muscle and composed of three bundles: subcutaneous, superficial, and deep.
- Subcutaneous External Sphincter: The lowest part of the external anal sphincter surrounds the anal canal outlet and is very close to the perianal skin.
- Superficial External Sphincter: It is above the subcutaneous part and under the deep part. Posteriorly, it attaches to the anococcygeal ligament attached to the coccyx.
- Deep External Sphincter: It is the uppermost part of the external anal sphincter. There are two different views regarding this muscle. According to some, the lower fibers of the puborectalis muscle make up the deep external sphincter. According to others, it is the puborectal muscle itself.
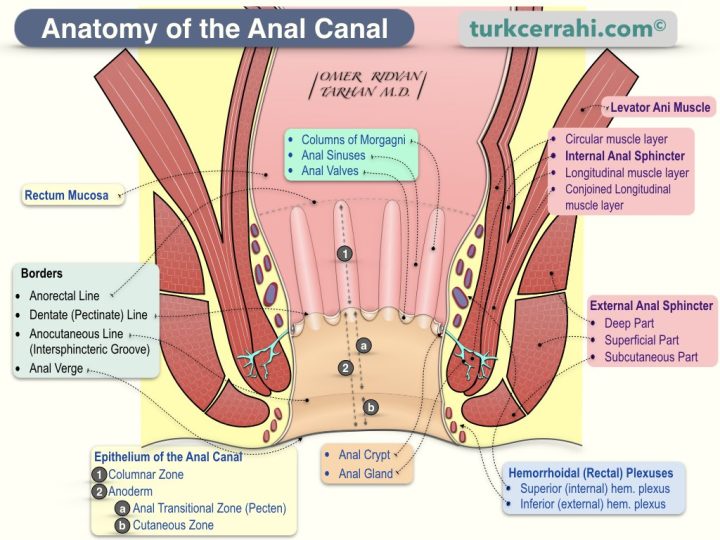
Inner Surface and Epithelium of the Anal Canal
The anal canal originates from the hindgut (endoderm) above the dentate line. Below the dentate line, it originates from the proctodeum (ectoderm). In other words, there is a transition from the gastrointestinal mucosa to the skin in the anal canal. The anal canal develops from the proctodeum (anal pit), which is an ectodermal depression at the embryo's caudal end.
The epithelium of the anal canal is divided into three distinct zones from top to bottom. .
1. Columnar Zone (Upper Zone): It is lined with columnar epithelium that is continuous with the lining of the rectum. This zone has longitudinal mucosal folds called anal columns (columns of Morgagni, 6–10 pieces). The groove-shaped depressions between the columns of Morgagni are called anal sinuses (Morgagni sinus, rectal sinus). The columns of Morgagni are connected at their lower edges by crescent-shaped mucosal folds (also called anal valves, semilunar valves, and transverse plicae). Anal valves are more prominent in children and obscured in adults. Behind each anal valve is an anal crypt, a bird's nest-shaped depression (anal crypt). In other words, the anal sinuses end with the anal crypt. Anal glands open into anal crypts. The anal glands secrete a lubricating mucus that facilitates defecation. This mucus is poured into the anal canal while straining during defecation. Anal crypts are the starting point of some perianal abscesses and fistulas. Cryptitis > cryptoglandular abscess > perianal abscess > fistula
Anal valves form a line of comb-like teeth called the pectinate line or dentate line (pectinate: comb-like, dentate: toothed edge).
2. Anal Transitional Zone (Anal Pecten): The mucosa between the dentate and anocutaneous lines. It is the nonkeratinized stratified squamous epithelium. It is sensitive like skin, with tactile and nociceptive (pain, itch) receptors (the inferior rectal (pudendal) nerve). That’s why an anal fissure is very painful, and the stitches in this area cause pain. The anal transitional zone has melanocytes, but it doesn't have hair, sweat glands, or sebaceous glands, which are all parts of normal skin (skin appendages).
3. Cutaneous Zone (Lower Zone): The part between the white line and the anal verge. The cutaneous zone is lined with squamous epithelium that is similar to the skin (keratinized stratified squamous epithelium). It contains all of the skin's appendages (pigment, hair, sweat glands, and sebaceous glands).
Anal Channel Encyclopedia
Anus
The anus is an opening at the end of the digestive tract where solid wastes are expelled from the body. It consists mainly of the anal canal and the sphincters surrounding the anal canal.
Surgical Anal Canal
The surgical anal canal starts from the levator ani muscle (or the anorectal junction, or the anorectal ring, or where the rectal ampulla ends and narrows) and ends at the anal verge.
Anatomical Anal Canal
The anatomical anal canal starts from the dentate line and ends at the anal verge.
Dentate Line (Pectinate Line)
Anal valves form a line of comb-like teeth called the pectinate line or dentate line (pectinate: comb-like, dentate: toothed edge).
Anocutaneous Line (Intersphincteric Groove, White Line, Hilton's White Line)
The anocutaneous line is the lower border of the anal pecten. It is located at the level of the lower edge of the internal anal sphincter. After this line, the anal pecten, which is hairless anoderm and stratified squamous epithelium, transforms into normal skin, which has hair.
Anal Verge (Anal Margin)
The anal verge is the edge where the anal canal ends. It is the border between the epithelium of the anal canal and the perianal skin.
Anoderm
Anoderm is the part of the anal canal between the pectinate (dentate) line and the anal verge (margin). The inferior rectal (pudendal) nerve innervates the anoderm. Tactile and nociceptive (i.e., pain and itch) receptors are abundant. It is prone to mechanical and chemical irritation, like rough toilet paper and soap. This area is prone to mechanical and chemical irritants, such as rough toilet paper and soap.
Anal Pecten
The anal pecten lies between the pectinate line and the intersphincteric groove and is the upper part of the anoderm. From another point of view, it is the middle third of the surgical anal canal and the upper half of the anatomical anal canal.
Columns of Morgagni (Anal Colons, Rectal Colons)
Columns of Morgagni are vertical mucosal folds in the upper part of the anal canal (columnar zone, in the form of a ridge). Between the anal columns, there are anal sinuses (in the form of a groove).
Morgagni Sinuses (Anal Sinus, Rectal Sinus)
Morgagni sinuses are the grooves between the columns of Morgagni in the upper part of the anal canal (in the columnar zone). They end with the anal crypt and anal valve.
Anal Crypts
Anal crypts are pocket-like recesses at the end of the anal sinus. Anal crypts lie behind the anal valves. In other words, the anal valve forms the wall of the anal crypt that faces the inside (center) of the anal canal. The anal glands open into this pocket (the anal crypts).
Anal Glands
Anal glands are located in the wall of the anal canal and open into anal crypts (via anal ducts) at the level of the dentate line. The anal glands secrete lubricating mucus into the anal canal during defecation. The anal glands lie at different depths in the anal canal wall. Some glands extend between the internal and external sphincters (intersphincteric plane). The cryptoglandular theory says that when the ducts of the anal glands are blocked (by a fecalith), this leads to cryptitis, which leads to a cryptoglandular abscess, which leads to a perianal abscess and fistula.
Anal Valves
Anal valves are small mucosal folds located at the bottom of the anal sinuses. The anal valves are like small curtains between the lower ends of the anal columns. In other words, anal valves connect the lower ends of the anal columns. There are anal crypts behind the curtains (valves).
Anal Papilla (Hypertrophied Anal Papilla)
According to some sources, the lower end of the anal columns looks like a papilla and is called the "anal papilla" as a normal part of the body. However, usually, the term "anal papilla" is used to mean "hypertrophic anal papilla." When the anal papilla is hypertrophied, a polypoid appearance occurs. The hypertrophic anal papilla is one of three signs of chronic anal fissure. The other two signs are chronic fissures with deep, raised edges that don't heal and show the muscle fibers of the internal anal sphincter underneath and skin tags at the end of the fissure.
Transitional Epithelium (Transitional Zone, Pecten)
The transitional epithelium is the mucosa between the dentate and anocutaneous lines. It is the nonkeratinized stratified squamous epithelium. Pecten is sensitive, like skin. It has receptors for touch (tactile receptors) and pain and itching (nociceptive receptors) and is connected to the inferior rectal (pudendal) nerves. That’s why an anal fissure is very painful, and the stitches in this area cause pain. The anal transitional zone has melanocytes, but it doesn't have hair, sweat glands, or sebaceous glands (skin appendages) like normal skin does.
3. Pelvic Floor and Pelvic Diaphragm
The pelvic floor is predominantly composed of muscles and connective tissue and separates the pelvic cavity from the perineum.
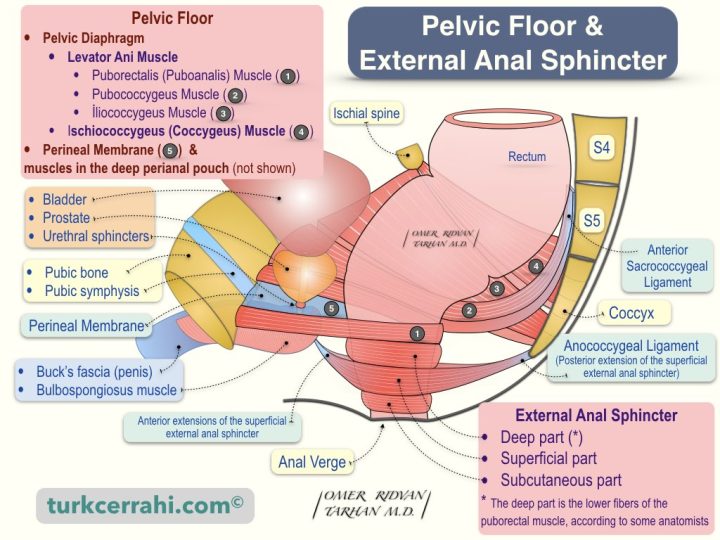
Structures that form the Pelvic Floor
- Pelvic Diaphragm: It is similar to a bowl or funnel.
- Levator Ani Muscle: Consists of three muscles from the outside to the inside
- Iliococcygeus Muscle: Actually, it does not attach to the ilium bone itself. It starts from the tendinous arch (origin) in the middle of the obturator internus muscle, which covers the inner surface of the os ilium and the obturator foramen. It enters the anococcygeal ligament in the posterior midline (insertion). The anococcygeal ligament (raphe) is a ligamentous structure that connects the levator ani muscles to the posterior margin and extends between the anal aperture and the coccyx.
- Pubococcygeus Muscle: It starts from the pubis body (origin), ends posteriorly, and in the midline, at the anococcygeal ligament and coccyx (insertion). The Pubococcygeus muscle lies between the iliococcygeus and puborectalis muscles.
- Puborectalis Muscle: It starts from the pubis body (origin), turns behind the rectum, and ends in the pubis body again. The puborectal muscle hangs the rectum anteriorly and creates the anorectal angle (also known as perineal flexure or anorectal flexure). The puborectalis muscle is at the level of the anorectal junction.
- Coccygeus Muscle (Ischiococcygeus Muscle): This triangular-shaped muscle forms the posterior portion of the pelvic diaphragm. The Coccygeus muscle starts from the ischial spine and the sacrospinous ligament (origin) and ends laterally in the coccyx and sacrum (insertion).
- Levator Ani Muscle: Consists of three muscles from the outside to the inside
- Perineal Membrane and Muscles in the Deep Perianal Pouch (Anterior Midline): The perineal membrane is a thick fascia that lies (attached) between both pubic arches. The ureter passes through the middle of this fascia, and the vagina passes behind the ureter (in women). The penis root is also attached to the lower surface of the perineal fascia.
4. Arteries of the Rectum and Anal Canal
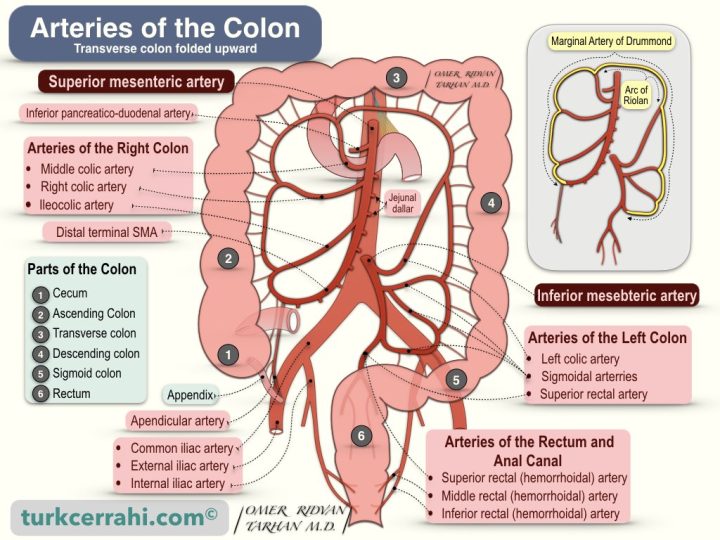
Superior Rectal (Hemorrhoidal) Artery
The superior rectal artery is the terminal branch of the inferior mesenteric artery. The superior rectal artery descends into the pelvis in the sigmoid mesocolon medially. It divides into two branches at the S3 vertebra and descends to the internal anal sphincter by giving small branches along the right and left sides of the rectum. The superior rectal artery supplies the proximal part of the rectum.
Middle Rectal (Hemorrhoidal) Artery
The middle rectal artery is a branch of the internal iliac artery. It supplies the distal rectum.
Inferior Rectal (Hemorrhoidal) Artery
The internal pudendal artery is the terminal branch of the anterior trunk of the internal iliac artery. The inferior rectal artery is a branch of the internal pudendal artery. It supplies the anal canal, the external anal sphincter, and the gluteal skin surrounding the anus.
There is a well-developed network connecting the terminal branches of the superior, middle, and inferior rectal arteries. This vascular network makes the rectum resistant to ischemia.
5. Veins of the Rectum and Anal Canal
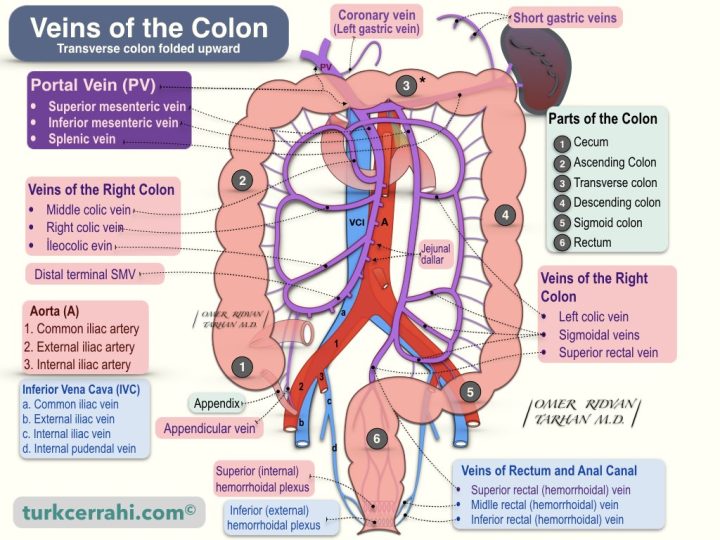
Superior Rectal (Hemorrhoidal) Vein
The superior rectal vein drains the proximal and distal rectum (via the superior (internal) hemorrhoidal plexus). The inferior mesenteric vein begins in the rectum as the superior rectal vein. The superior rectal vein is also called the superior anorectal vein.
Middle Rectal (Hemorrhoidal) Vein
The middle and inferior rectal veins together drain blood from the anal canal, anal muscles, and surrounding gluteal skin (via the inferior (external) hemorrhoidal plexus). The middle rectal vein joins the internal iliac vein. The middle rectal vein is also called the middle anorectal vein.
Inferior Rectal (Hemorrhoidal) Vein
The inferior rectal vein and the middle rectal vein drain blood from the anal canal, the anal muscles, and the skin around the gluteal area (via the inferior (external) hemorrhoidal plexus). The inferior rectal vein is also called the inferior anorectal vein.
The inferior rectal vein begins with several branches and drains into the internal pudendal vein. After getting the middle rectal vein and some other small veins, the internal pudendal vein turns into the anterior branch of the internal iliac vein.
Rectal Venous Plexus (Hemorrhoidal Plexus)
The veins draining the distal rectum and the anus arise from two venous plexuses.
- Internal (superior) hemorrhoidal (rectal) plexus
- External (inferior) hemorrhoidal (rectal) plexus
In portal hypertension, the connections between the superior and inferior hemorrhoidal plexuses enlarge and act as portosystemic collaterals.
The internal hemorrhoidal plexus is located submucosal and just above the anorectal line. It drains into the superior hemorrhoidal (rectal) vein > inferior mesenteric vein > portal system.
Dilatation and elongation of the internal hemorrhoidal veins cause internal hemorrhoid disease. Portal hypertension is precisely reflected in the internal hemorrhoid plexus because the caval vessels lack venous valves. Therefore, there is a tendency to develop internal hemorrhoidal disease.
The external hemorrhoidal plexus is located outside the muscular layer and lies below the anorectal line, drains into two veins
- Inferior hemorrhoidal (rectal) vein > internal pudendal vein > internal iliac vein > caval system
- Middle hemorrhoidal (rectal) vein > internal iliac vein > caval system
Enlargement of the external hemorrhoidal plexus causes external hemorrhoidal disease.
6. Lymphatic Drainage of the Rectum and Anal Canal
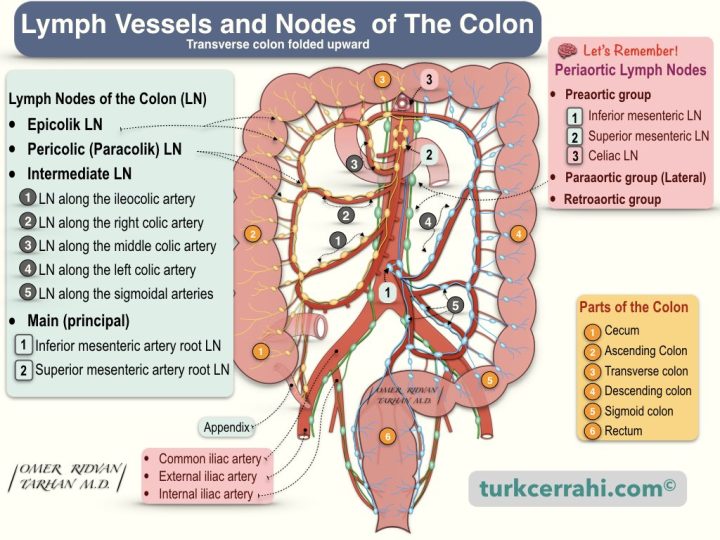
The lymphatic drainage of the rectum is parallel to the arteries.
- The lymphatics of the upper and middle rectum drain upward into the inferior mesenteric lymph nodes.
- The lymphatics of the lower rectum drain both upward (into the inferior mesenteric lymph nodes) and laterally (into the internal iliac lymph nodes).
The anal canal has a more complex lymphatic drainage pattern.
- Proximal to the dentate line, lymphatic drains into both the inferior mesenteric lymph nodes and the internal iliac lymph nodes.
- Distal to the dentate line, lymphatic primarily drains into the inguinal lymph nodes, but may also drain into the inferior mesenteric lymph nodes and internal iliac lymph nodes.
7. Innervation of the Rectum and Anal Canal
Both sympathetic and parasympathetic nerves innervate the anorectum.
Sympathetic nerve fibers come from L1–L3 and join the preaortic plexus. The preaortic nerve fibers then go below the aorta to form the (superior) hypogastric plexus. Fibers of the hypogastric plexus converge to form the hypogastric nerve. The hypogastric nerve then divides into fibers and connects to the parasympathetic nerves (nervi erigentes = pelvic splanchnic nerves) to form the pelvic plexus.
Parasympathetic nerve fibers (pelvic splanchnic nerves) are called nervi erigentes and originate from S2–S4. These fibers join the sympathetic fibers to form the pelvic (inferior hypogastric) plexus. Sympathetic and parasympathetic fibers then supply the anorectum and adjacent urogenital organs.
The internal anal sphincter is innervated by sympathetic and parasympathetic nerve fibers. Both types of fibers inhibit sphincter contraction. The external anal sphincter and puborectalis muscles are innervated by the inferior rectal branch of the internal pudendal nerve.
The levator ani receives innervation from both the internal pudendal nerve and branches from S3 to S5.
The sensory innervation of the anal canal is supplied by the inferior rectal branch of the pudendal nerve. The anal canal below the dentate line receives somatic innervation, while the rectum is relatively insensitive.
8. Differences in the Anal Canal Above and Below the Dentate Line
The dentate line, also called the pectinate line, is the embryological junction of the hindgut and the proctodeum. Therefore, the dentate line is an important anatomical boundary, with many anatomical and histological differences above and below this line.
| Above the Dentate Line | Below the Dentate Line | |
|---|---|---|
| Embryological Origin | Endoderm (Hindgut) | Ectoderm (Proctodeum) |
| Epithelium | Simple columnar epithelium | Stratified squamous epithelium |
| Arterial Supply | Inferior mesenteric artery > Superior rectal artery | Internal iliac artery > middle and inferior rectal artery |
| Venous Drainage | Superior rectal vein > inferior mesenteric vein > portal system | Middle and inferior rectal vein > internal iliac vein > systemic circulation |
| Lymphatic Drainage | Internal iliac lymph nodes | Superficial inguinal lymph nodes |
| Innervation (Nerves) | Inferior hypogastric (pelvic) plexus (autonomic fibers (visceral)) | Inferior rectal (pudendal) nerves (somatic) |
| Sensation | It is not sensitive | Sensitive like skin, with tactile and nociceptive (pain, itch) receptors |
| Hemorrhoid Type | Internal hemorrhoids | External hemorrhoids |
| Cancer Type | Adenocarcinoma | Squamous cell carcinoma |
9. Defecation Physiology
The stool coming from the sigmoid colon is stored in the rectum before defecation. Rectal distension induces a temporary relaxation of the internal anal sphincter, known as the rectoanal inhibitory reflex (RAIR). RAIR allows a small amount of content to make contact with the anal canal. Therefore, RAIR is also called the anal sampling mechanism, anal sampling reflex, rectosphincteric reflex, or anorectal sampling reflex. The sensory epithelium of the anal canal determines the composition of the rectal contents (gaseous, liquid, or solid).
If a person is unwilling to defecate, voluntary contraction of the external anal sphincter can delay defecation. The stool returns to the sigmoid colon, and the water in the stool continues to be absorbed, causing it to harden even more.
If the decision is to defecate, the person first sits or squats. Sitting or squatting widens the anorectal angle. Then, straining and simultaneously relaxing the external and internal anal sphincters and puborectalis muscle as a reflex will cause the body to expel feces. Straining also causes the pelvic floor to descend, forming a funnel. The contraction and shortening of the rectum during defecation may also contribute to the process. Sometimes defecation can occur without straining.
Following defecation, the external anal sphincter regains tone to maintain continence during rest (closing reflex).