Operating Room
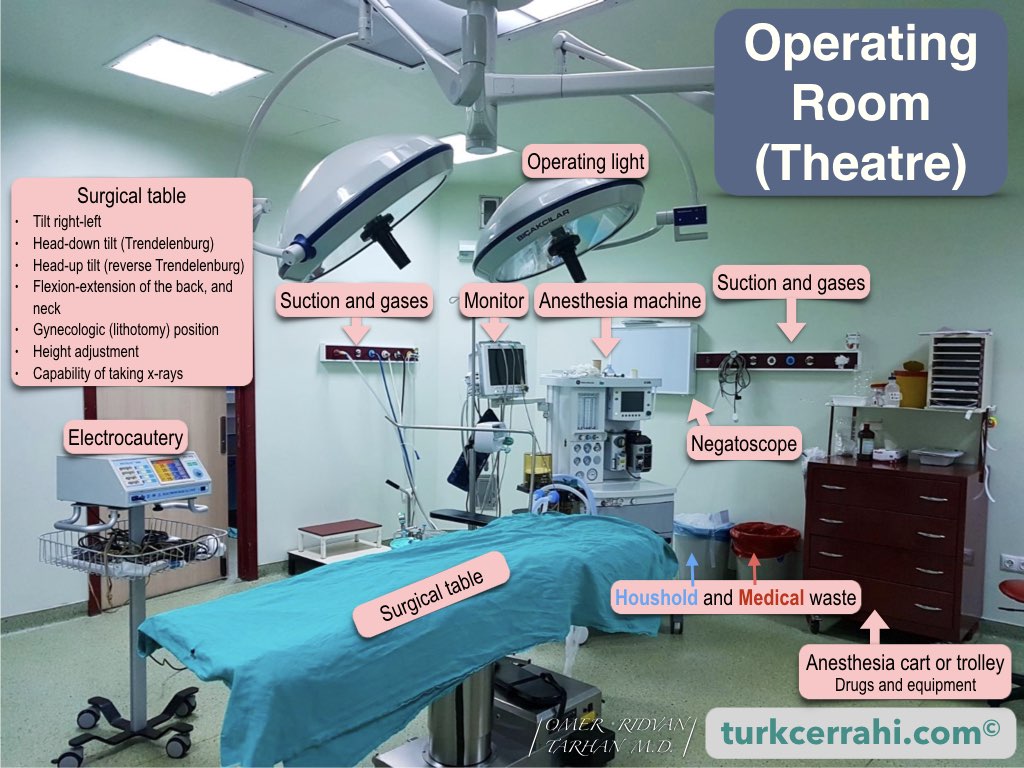
The operating room or theater (American English) or operating theatre (British English) is a sterile environment within a hospital where surgical procedures take place. An operating suite contains multiple operating theaters.
The operating rooms are spacious (large), well-lit, and easy to clean. They typically do not have windows, or if they do, the windows are limited by a wall. The humidity and room temperature are controlled by the ventilation system.
Operating Room Equipment
The main equipment found in the operating room includes the operating (surgical) table and anesthesia machine. Additionally, there are tables for sterilized surgical instruments and cabinets for shared surgical supplies. There are special sinks for surgical handwashing located near the entrance of the operating room, which are usually equipped with touchless or foot-operated faucets. Hands are washed with antiseptic soap for this purpose.
Surgical Tables
The surgical table is usually located in the middle of the room and can be adjusted for height, rotation, and flexion of the hips, back, and neck. The table can be tilted with the feet up (Trendelenburg) or down (reverse Trendelenburg) to provide different angles. The lower parts of the surgical table legs can be removed, and special stirrups can be attached to provide gynecological (lithotomy) positioning for the patient (also called the lithotomy position). Many surgical tables have the capability of taking x-rays and performing endoscopic procedures.
Operating Room Lightning
The surgical or operating light in the operating room is a powerful light designed to provide illumination without creating shadows. They consist of multiple lamps arranged in a large circle, all focused on a single point to prevent shadows. Each operating light has a sterile handle that can be adjusted by the surgical team. The surgical light can be moved in any direction (horizontally and vertically) and can be tilted in all directions.
Anesthesia Machine
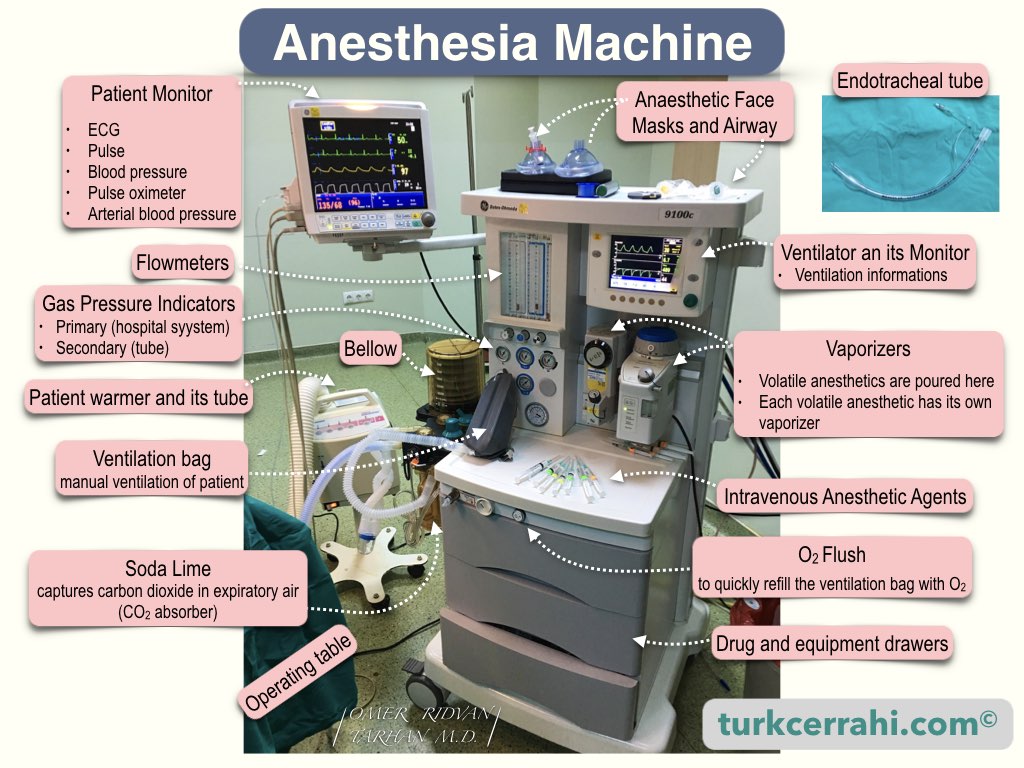
The anesthesia machine (American English) or anaesthetic machine (British English) is located at the head of the surgical table. This machine is used to help the patient breathe during surgery and delivers anesthetic gases and oxygen to the patient. The machine has internal monitors to help control the gas mixture in the breathing tubes and respiratory circuit. A special monitor is part of the anesthesia machine and displays the following information:
- Electrocardiogram (ECG) readings, which continuously monitor the patient’s heart rate and rhythm
- Real-time respiratory rate
- Oxygen saturation, which is measured using a pulse oximeter attached to the patient’s finger
- Blood pressure, which can be measured using an automatic blood pressure cuff that can be timed or manually initiated
- Arterial blood pressure, which can be monitored in real-time if an arterial catheter has been inserted (usually into the radial artery)
The anesthesia machine is often accompanied by an anesthesia cart or trolley, which holds the drugs and equipment that the anesthesiologist may need during the procedure.
Surgical Instrument Table
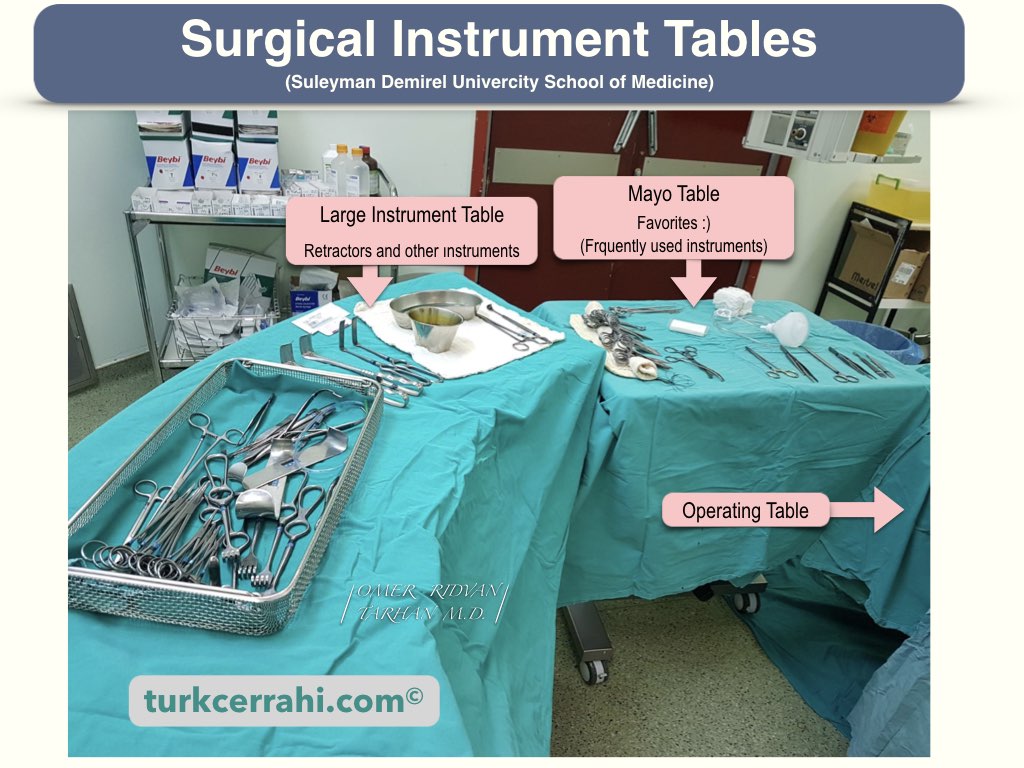
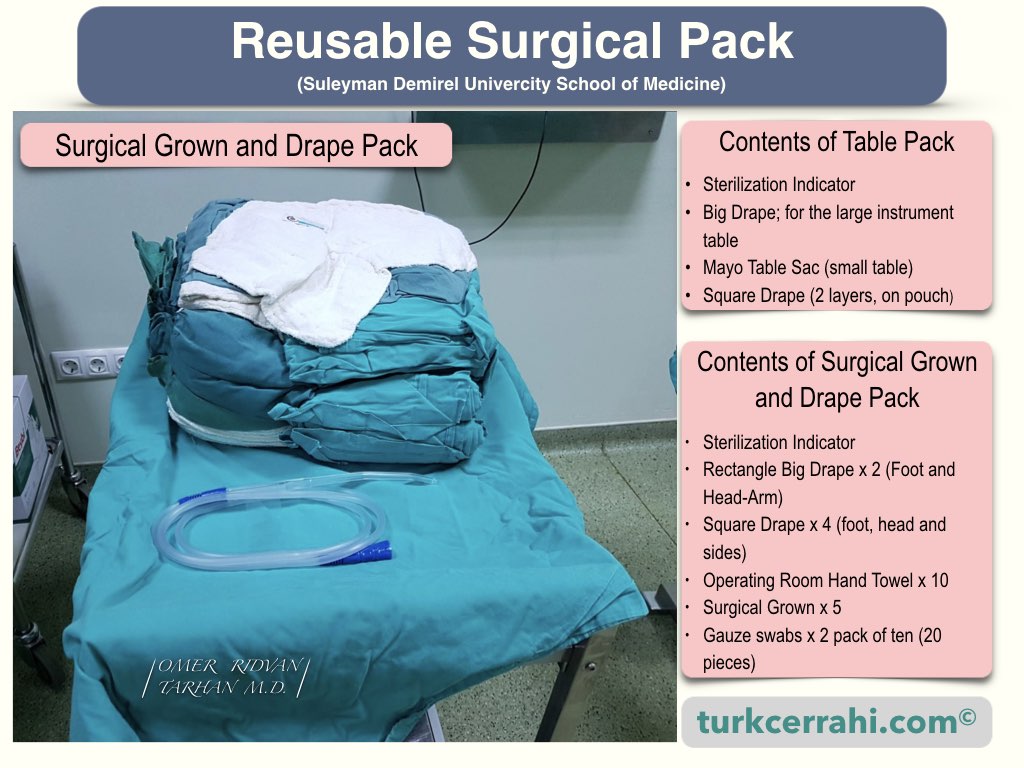
Sterile instruments to be used during surgery are placed on a stainless steel table covered with a sterile drape. During the operation, it is brought closer to the surgical table.
Electrocautery Machine
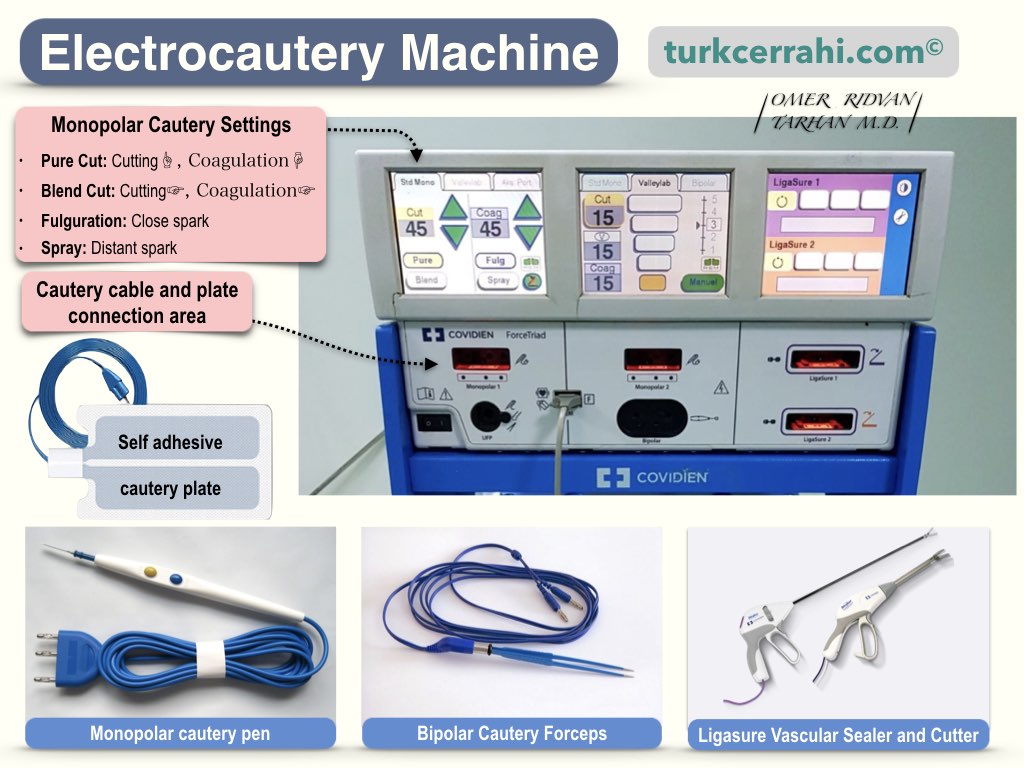
A cautery pen is an electric tool with a pen-like tip that burns and cuts tissues, allowing for bloodless surgery. There are two main types of electrocautery:
- Unipolar (monopolar) electrocautery
- Bipolar electrocautery
Monopolar cautery: Tissue is touched with a single electrode. The output point of the circuit is the wide-surfaced cautery plate, which is attached to the thigh, hip, or back.
Bipolar cautery: Electricity passes from one jaw to the other of a bipolar forceps or bipolar scissors. Therefore, there is no need to attach a cautery plate to the patient. Since there is no electric current flowing through the body, it does not affect the rhythm and function of the heart or a possible pacemaker.
Who Works in the Operating Room?
Surgeon
The surgeon performs or oversees the surgery (medical school and teaching hospitals).
Registered Nurse First Assistant (RNFA)
The RNFA assists the surgeon. This is sometimes another surgeon, sometimes a surgery resident who has received surgical training, sometimes a medical student, or sometimes an operating room nurse.
Scrub Nurse
After the sterile garments and drapes are unpacked, the scrub nurse is the first to dress in sterile attire, set up the surgical instruments on the surgical instrument table, and help the others dress. Throughout the surgery, the operating room nurse gives the surgeon the surgical instruments he or she needs and cleans them as necessary. A scrub nurse who works in harmony with the surgeon ensures that the work is smooth and reduces the tension of the surgery.
Medical Student
Sometimes he or she assists the surgeon in the operation, pulls the retractors, is assigned tasks such as suturing or cutting threads, or simply observes. Sometimes a medical student observes without being sterile. For most medical students, participating in surgery, especially for the first time, is a unique experience. Sometimes, putting in a single stitch can be just as satisfying as performing a major surgery.
Anesthesiologist
The anesthesiologist stands at the head of the patient and is responsible for administering anesthesia with intravenous (IV) anesthetics and gases, intubating (general anesthesia), and sometimes applying spinal-epidural anesthesia or nerve blocks (regional anesthesia).
Throughout the operation, the anesthesiologist monitors the patient’s hemodynamics, administers fluids and, if necessary, blood replacement, and maintains anesthesia. In general anesthesia, the patient’s induction and recovery, like the takeoff and landing of an airplane, are two critical stages. The anesthesiologist and surgeon working in harmony can make the surgery easier, but discord can put the surgeon in a difficult position.
Anesthesiologist Assistant
Certified anesthesiologist assistants (CAAs) are non-physician anesthetists. All certified anesthesiologist assistants have premedical backgrounds, baccalaureate degrees, and master’s degrees from accredited anesthesia programs. The anesthesiologist assistant helps the specialist anesthesia doctor in the anesthesia process before surgery. They prepare the necessary materials, drugs, and anesthesia machines. They participate in patient monitoring at the start of anesthesia, during anesthesia, and at the end of anesthesia.
Surgical technologist
They prepare the operating room and table in terms of materials and equipment. They send pathology cultures and other samples to the relevant unit. After surgery, they clean and disinfect the operating room. They clean surgical instruments and materials. They assist in positioning the patient in the operating room and in transporting them after surgery. During surgery, they assist the surgical team in the manner deemed appropriate by the physician (supplying and opening sterile instruments).

Features of the Operating Room
Dimensions
While the required dimensions may vary, the recommended size is 6.5 m x 6.5 m x 3.5 m. If there is to be a window, it can only be planned on one side.
Doors
The main door should have a minimum width of 1.2 – 1.5 m. Swinging doors can be used, but automatic sliding doors are preferred. The connecting elements and other parts on the door should be made of stainless steel.
Flooring and Walls
The floor should be non-slip, sturdy (against chemicals and disinfectants), and have minimal seams. The walls can be covered with laminated polyester or a non-glossy paint. Tiles can break, and epoxy paint can peel, so they should not be used. Corners and edges should be covered with steel or aluminum borders, or the flooring should be curved in a way that does not create corners toward the wall.
Ventilation
Ventilation of the operating room is applied in a form called laminar flow. Here, continuously filtered clean air is supplied to the operating room, and a continuous positive pressure of at least 5 cm H2O is created in the room so that the airflow constantly flows from inside the room to the outside. This minimizes potential contamination from the air. The air in the operating room should change 20-30 times per hour, and at least 90% of particles 0.5 microns or larger should be filtered. The humidity in the operating room should be between 40-60% and the temperature should be between 20-24°C. The temperature of the operating room should be adjusted according to the patient, not the staff (e.g., child, newborn, elderly, burn patient, etc.).
Electrical System
Operating room is connected to an uninterrupted power supply (battery) and a generator system. Each operating room has an aspirator system and an oxygen system.
« Return to Dictionary